Therapeutic Ultrasound for treatment of Blocked Breast Ducts
By Agnes Budyn, Registered Physiotherapist PT, pelvic health certified
Breastfeeding can be a wonderful way of feeding and connecting with your baby. And while there are a lot of benefits to it, there are also a lot of challenges that women often experience. One common challenge is a clogged milk duct which can happen at any point in a woman’s breastfeeding/pumping journey.
Blocked ducts can cause discomfort, and pain, and even lead to more serious complications like mastitis if left untreated.
While traditional remedies often involve warm compresses, massage, or manual expression, there’s a growing interest in therapeutic breast ultrasound as a non-invasive treatment option. In this post, we’ll explore how therapeutic breast ultrasound works, its benefits, and why it might be the right treatment for blocked ducts.
What is a Blocked Milk Duct?
A blocked milk duct occurs when milk flow is obstructed in one of the milk-producing glands of the breast. This typically happens when milk is not fully expressed, causing a buildup that can lead to swelling, pain, and even hard lumps in the breast. Blocked ducts are common in the early stages of breastfeeding, particularly if the baby isn’t latching properly or the breast is not emptied completely during nursing but can happen at any time.
Common symptoms of a blocked duct can include:
- A lump over the area of the breast where there is a build-up of milk
- Slower flow or a decrease in milk supply can be common on the affected side
- Warmth or redness may be present over the affected area accompanied by pain
If a blocked duct is left untreated, it can lead to inflammation and infection, resulting in mastitis — a painful condition that often requires antibiotics. Therefore, it’s important to address a blocked duct as soon as symptoms arise.
Traditional Treatments for Blocked Ducts
The most common treatments for blocked ducts include:
- Warm compresses: Applying heat to the affected area can help loosen the blockage and encourage milk flow.
- Gentle massage: Massaging the breast while nursing or pumping can help to manually express milk and relieve the blockage.
- Frequent feeding or pumping: Ensuring the baby nurses frequently or pumping the affected breast can help to clear the duct and relieve pressure.
- Position changes during nursing: Different breastfeeding positions can sometimes help to target the area of the blockage more effectively.
However, these methods are not always effective on their own or may take too long to work. This is where therapeutic breast ultrasound comes in.
What is Therapeutic Breast Ultrasound?
Therapeutic breast ultrasound is a conservative treatment that uses sound waves and gentle heat to stimulate the breast tissue and help relieve blocked ducts, kind of like a mini massage to the area! The procedure is often used in physical therapy and has been adapted for blocked ducts where the treatment is performed directly to the affected area on the breast. The vibrations caused by the sound waves can help to break up the blockage by promoting circulation, reducing inflammation, and encouraging milk flow. The treatment is gentle, typically taking about 10-15 minutes per session, and can be done in conjunction with other breast care techniques.
Benefits of Therapeutic Breast Ultrasound for Blocked Ducts
- Effective and Non-Invasive: Ultrasound therapy is non-invasive and generally considered safe for breastfeeding mothers. It offers a gentle solution that can be used alongside other methods like breastfeeding or pumping.
- Pain Relief: The soothing effects of ultrasound waves can help alleviate the discomfort and pain associated with blocked ducts, allowing mothers to feel more comfortable while continuing to care for their baby.
- Faster Recovery: Ultrasound therapy can help clear the blockage more quickly than manual techniques, potentially reducing the risk of developing mastitis or other complications.
- No Need for Medication: For mothers who wish to avoid medication or antibiotics, therapeutic ultrasound can be an appealing alternative to address the blockage before it develops into a more serious issue, like an infection.
Is Therapeutic Breast Ultrasound Right for You?
Therapeutic ultrasound can be an effective treatment for many women experiencing blocked ducts, but it’s important to consult with a healthcare provider before starting any treatment. A lactation consultant or a doctor/midwife can help determine if this approach is right for you based on the severity of your blockage and your overall health.
Blocked milk ducts can be a painful and frustrating experience for nursing mothers, but therapeutic breast ultrasound offers a promising, conservative solution to relieve the condition. By promoting circulation, reducing inflammation, and helping to clear the blockage, ultrasound therapy can provide much-needed relief and help mothers continue breastfeeding/pumping comfortably.
If you’re struggling with blocked ducts, consider talking to your healthcare provider about whether therapeutic breast ultrasound could be a beneficial addition to your treatment plan. As always, seek professional advice and support when managing breastfeeding-related concerns to ensure both you and your baby’s health and well-being.
If you are experiencing blocked ducts or want to find out more, please reach out to Agnes, registered physiotherapist, specializing in pelvic health for more information. Click here to book Agnes Budyn:
 Agnes Budyn
Agnes Budyn
Physiotherapist – DPT, PT, BSc (Hons) Life Sci
Agnes Budyn is an experienced Pelvic Health Physiotherapist with a special interest in pre and post natal woman’s health. She is now offering Therapeutic Breast Ultrasound at Synergy Sports Medicine and Rehabilitation located at 2155 Danforth Avenue, Toronto.

 Agnes Budyn
Agnes Budyn
 Jarod Roy
Jarod Roy












 Rachel Varga
Rachel Varga


















 Leah Forrestall
Leah Forrestall Samy Shash
Samy Shash I refer to this muscle as a real pain in the butt, as it can often be the source of a lot of discomfort in the area. One particular condition this muscle can lead to is Piriformis Syndrome.
I refer to this muscle as a real pain in the butt, as it can often be the source of a lot of discomfort in the area. One particular condition this muscle can lead to is Piriformis Syndrome.
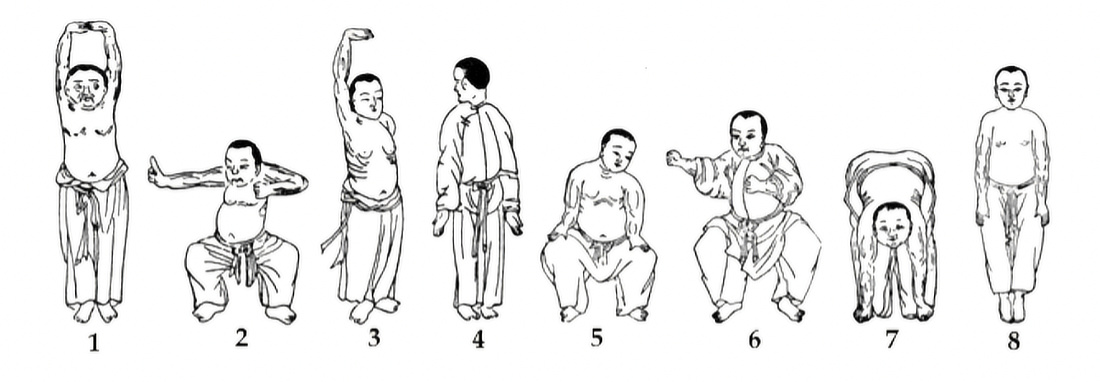
 Position yourself lying down on your back. Keep the non-exercising leg straight, as you bring your exercising knee to your chest. Then, pull your foot toward your opposite hip.
Position yourself lying down on your back. Keep the non-exercising leg straight, as you bring your exercising knee to your chest. Then, pull your foot toward your opposite hip. Position yourself lying down on your back with both knees bent. Cross your exercising leg over the non-exercising leg to rest your ankle on the opposite thigh. Then, gently push the exercising knee downward and away from your body.
Position yourself lying down on your back with both knees bent. Cross your exercising leg over the non-exercising leg to rest your ankle on the opposite thigh. Then, gently push the exercising knee downward and away from your body.









 Rebecca Watson
Rebecca Watson





















